Keratoconus Treatment


What is Keratoconus?
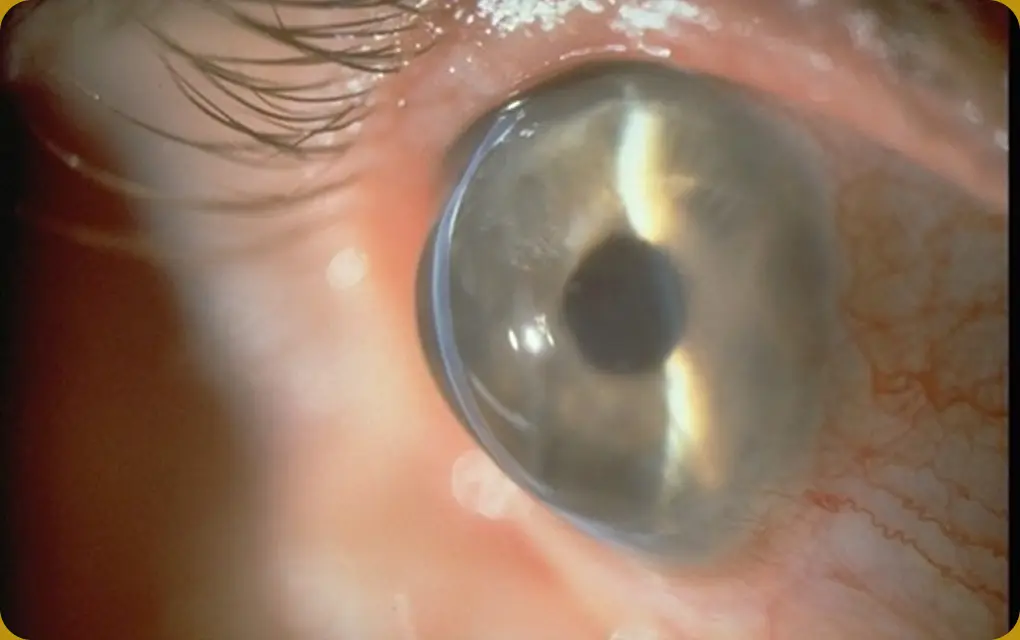
The term keratoconus originates from two Greek words: kerato, meaning cornea, and konos, meaning cone. Keratoconus is a condition in which the cornea gradually becomes thinner and begins to bulge outward into a cone shape. This deformation typically leads to decreased vision and the development of astigmatism. The onset of symptoms varies depending on age, but the earlier the condition begins, the faster it tends to progress. Keratoconus usually affects both eyes, although the degree and shape of the deformation are often asymmetrical between the two eyes.

Causes of
Keratoconus
The exact cause of keratoconus is still not fully understood, but it is believed to have a genetic component. It often appears as a form of skip- generation inheritance, where a trait found in ancestors may reappear in later generations. Keratoconus typically begins during puberty and is often associated with allergies. In particular, many patients also have atopic dermatitis. Frequent eye rubbing is thought to contribute significantly to the progression of the condition. These factors suggest that keratoconus develops due to a combination of genetic predisposition and environmental triggers. In Japan, it is estimated that keratoconus affects approximately 1 in every 1,000 to 2,000 people.
Symptoms of Keratoconus
-

Progressive Vision Decline
Nighttime vision may blur or distort, making glasses or contacts less effective.
-

Irregular Astigmatism
Objects may look wavy, with increased sensitivity to bright lights and glare.
-

Severe Eye Pain
In advanced stages, the thin cornea can rub against contact lenses, causing sharp pain and irritation, often making lens wear impossible.
-

Frequent Changes in
Glasses PrescriptionVision changes frequently, requiring constant updates to glasses or contact lenses.
-

Contact Lens Intolerance
Hard contact lenses may fall out or cause discomfort as the cornea becomes more cone-shaped and harder to fit.
-
Acute Hydrops
Severe cases can cause corneal tears, leading to pain, cloudiness, and swelling that may require urgent treatment or a transplant.

Diagnosis of
Keratoconus
Keratoconus is often mistaken for regular astigmatism in the early stages, making it difficult to diagnose with standard eye exams. However, early detection is very important because the condition can worsen and may eventually require a corneal transplant. Thanks to advances in technology, keratoconus can now be diagnosed more easily using specialized equipment. Unfortunately, not all clinics have these tools yet. At Eye Can, we use the latest diagnostic machines to detect keratoconus early, track its progression, and provide the right treatment at the right time.
What is Corneal Cross-Linking?
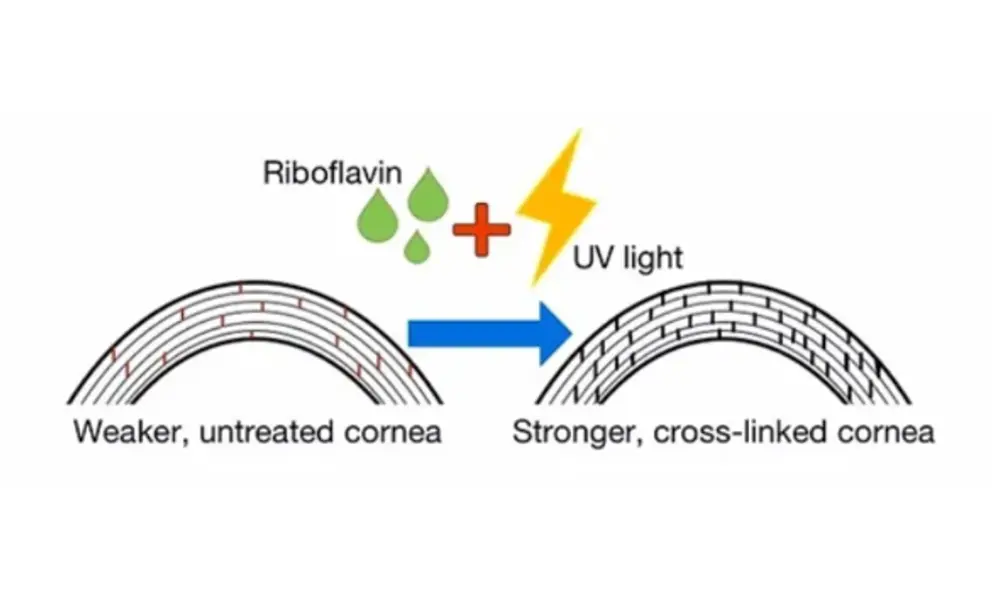
Corneal cross-linking (CXL) is a minimally invasive outpatient procedure that halts the progression of keratoconus by strengthening the cornea using UV light and riboflavin butyrate.
・Stabilizes the cornea・Prevents further vision deterioration
・Often avoids the need for corneal transplant
(About 99% of corneal transplants are due to keratoconus)
・90% success rate in stopping keratoconus progression
Is Cross-Linking Right for You?
It’s best to act early — cross-linking is most
effective when keratoconus is detected soon.
-

Keratoconus
-
Pellucid Marginal
Degeneration -

Post-LASIK
Certain Corneal -

Corneal Ectasia
Infections
Why Choose Eye Can
for Your Treatment?
-

Painless, non-surgical treatment
-

Prevent worsening vision
and stop keratoconus
from progressing -

Short recovery time
-

Led by experts
Treatment Process
Corneal topography and corneal thickness measurement.
Approximate duration: 60 minutes

Administer Topical Anesthesia (Eye drops)

Instill Riboflavin TE eye drops and wait for 40–50 minutes

Apply UV light for 6 minutes

Place soft contact lens on the eye to complete the procedure

Mild discomfort for 1–2 days

Use of eye drops and
follow-up checkups
for several weeks
Vision gradually stabilizes over time


